One of Palm Springs’ Top Doctors warns parents about a dangerous new trend targeting their children.
Many parents probably think JUUL is the new Candy Crush or Fortnite saga. But if you hear your teen talking about JUULing, you had better pay attention because they are talking about a new insidious way of smoking, or worse, getting high.
JUUL is a new type of e-cigarette whose main feature is discretion. Have you ever been waiting in traffic and see the car next to you suddenly fill with smoke? That’s an e-cigarette. With JUUL, the vapor is much less obvious allowing users to “vape” discreetly.
As someone who has walked through a plume of this noxious e-cigarette discharge, I say thank goodness as most e-cigarette users are unaware of the cancer-causing side effects they are blowing into public domain. But speaking as a parent this is very troubling.
E-cigarettes were originally developed to create a healthier alternative to smoking because the heat source is a battery rather than a flame, which reduces the smoker’s inhalation of nitrogen and other harmful chemicals. Hence why you “smoke” cigarettes but “vape” e-cigs. As a physician, I support this attempt to help wean adult smokers off cigarettes. But the slick design, fruity and sweet flavors and rebellious image that has always been associated with smoking makes vaping vastly more attractive to kids.
But that plume of e-cigarette vapor was a dead giveaway that something was amiss. With the JUUL e-cigarette, the vapor disappears in seconds. Students can discreetly take a puff and subtly blow it down their sleeve, often going unnoticed. And this is happening not only on the bus, but feet away from teachers in a classroom setting; completely inconspicuous and nearly impossible to reprehend.
Yes, e-cigarettes are less unhealthy than traditional cigarettes like getting hit by a car is less painful than getting hit by a truck. So let’s break down what is actually in e-cigarettes: nicotine, chemical flavorings, metals like lead, volatile organic compounds as well as other cancer-causing agents.
Nicotine is not only physically and psychologically addictive, but long-term exposure can have lasting effects on adolescent brain development, specifically in the areas that directly affect emotional and cognitive processing. The Center for Disease Control warns that “early exposure to nicotine during the transition from child to adult may be harmful, since it may derange the normal course of the brain maturation.”
And if you think this doesn’t apply to your non-vaping teen, you’re wrong. In 2016, the CDC reported more than 2 million U.S. middle and high school students used e-cigarettes in a 30 day span, including 4.3% middle school students and 11.3% of high school students. However, that figure balloons to 1 in 4 U.S. youths when you consider the effects of second-hand vapor. Contrary to popular opinion, e-cigarettes don’t just discharge water vapor, but also a potent cocktail of chemicals that others can be exposed to, similar to secondhand smoke.
One major misconception about lung cancer is that many people think it is a selfinflicted disease. As a thoracic surgeon, I can tell you this is not always the case. Up to 15% of lung cancer patients were never smokers but were exposed to airborne toxins such as those in secondhand smoke.
Then there are those chemicals used to create the JUUL flavors. While food flavorings are classified by the FDA as Generally Recognized As Safe (GRAS), that designation is for ingestion, not for inhalation. There is little published research on inhaling food flavorings, since the concept began with e-cigarettes just a few years ago. However, diacetyl and acetyl propionyl, chemicals used in the flavorings, have been shown to cause bronchiolitis obliterans, also known as popcorn lungs, which is a scarring of the tiny air sacs in the lungs resulting in the thickening and narrowing of the airways if inhaled in large enough quantities.
What many e-cigarette companies claim is that these devices are not intended for children or other non-smokers. They should only be used to help adults quit smoking. But we’ve been down this same road before with cigarettes. Companies claim they are marketing to adults and never intend to get children hooked, but inevitably, some do.
Teens favor JUUL because the nicotine content is high enough to experience a rush, stimulating the adrenal glands to release the hormone epinephrine and increases the levels of a chemical messenger in the brain called dopamine, while being small enough to hide from teachers and other students during class time.
According to JUUL Chief Administrative Officer Ashley Gould, the company’s main objectives are to “provide the 38 million American adult smokers with meaningful alternatives to cigarettes while also ensuring that individuals who are not already smokers, particularly young people, are not attracted to nicotine products such as JUUL.”
Kevin Burns, the Chief Executive Officer at JUUL, passionately states they are “committed to deterring young people, as well as adults who do not currently smoke, from using our products.” Burns says “we cannot be more emphatic on this point: no young person or nonnicotine user should ever try JUUL.”
So what can you do to keep your teens from vaping?
It may not seem like it, but we teach our children what is cool. And by “we,” I mean our society. We are a culture of conspicuous coolness, regardless of addiction. We clutch our iPhones the same way our parents clutched a pack of cigarettes 50 years ago. If our generation can signal to our children that addiction to anything – approval, technology, nicotine – is not a sign of strength or power, but of dependence, then they may possibly be able to resist the seductive pull of e-cigarette marketing and the peer pressure that inevitably follows. As a father, I try to educate my kids about those dangers and hopefully I inspire them to not only be nonsmokers but to also help their friends make the same choices.
If someone you know is already addicted to vaping, a simple yet powerful tool to help with the attempt to quit is to overload on lollipops. Every time the urge strikes, grab a lollipop to satisfy the oral fixation. To satisfy the nicotine addiction of the mind and body, use a nicotine patch. Taking these steps have a proven success rate.
Not only is education of the dangers and consequences of vaping crucial, but helping our youth develop the ability to delay their constant need for immediate gratification could help end this addictive trend, as we are slowly seeing with cigarettes. Many teens would never touch a cigarette, yet they think vaping and JUULing is cool and safe. Once again, it’s time to put the brakes on the marketing sensationalism so we do not create another regretful and unhealthy generation.
Let me be very clear – vaping puts our children at a higher risk of lung cancer and ultimately, death. We all take breathing for granted until we can’t. If we want to lift the vaping haze the future holds, be empowered by the facts and teach them to your children.
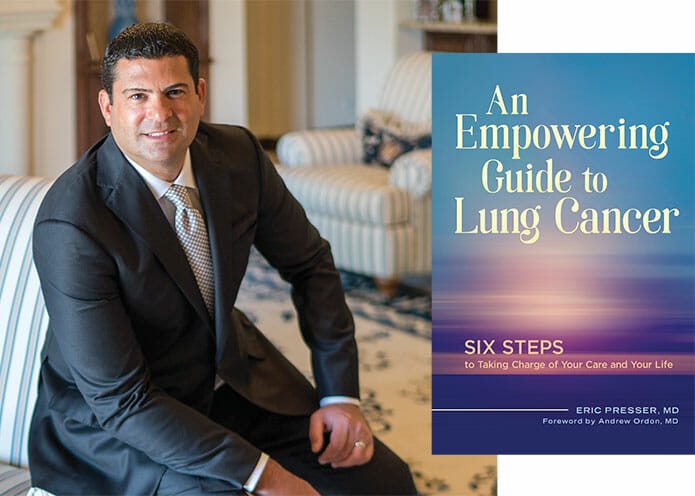
Medical School: M.D. Ross University School of Medicine
Internship & Residency: St. Vincent Hospital and Medical Center NY, New York
Cardiothoracic Fellowship: LSU Health Science and Medical Center, New Orleans, Louisiana; University of Texas Health Science Center (UTSA), San Antonio, Texas
Board Certifications: American Board of Thoracic Surgery
Special Interests: Minimally invasive lung and mediastinal surgery, adult thoracic surgery, thoracic surgical oncology
Hospital Affiliations: Desert Regional Medical Center; JFK Memorial Hospital
Professional Memberships: Society of Thoracic Surgeons; American Association of Thoracic Surgeons
Additional Information: Dr. Presser had resided in New York and was employed as a thoracic surgeon in both private practice and the North Shore LIJ Health System on Long Island since 2006. He has been in practice as an attending thoracic surgeon here in the Coachella Valley since May 2012. His knowledge in minimally invasive lung and mediastinal surgery with video assisted technology results in smaller incisions, less pain and stress on the body, with shorter recovery and hospitalization time.